The Gut-Brain-Liver Axis and the Lungs: How Imbalances Affect Your Breathing
When we think about our lungs, we often focus on things like air quality, exercise, or smoking. But did you know that your gut, brain, and liver are also deeply connected to your lung health? It’s true! These organs don’t just work in isolation—they’re part of a complex network that influences how well you breathe and how your body fights off infections. When this network gets out of balance, it can have a big impact on your lungs. Let’s dive into how this connection works and why it matters.
The Gut-Brain-Liver Axis: A Team Effort
Your gut, brain, and liver are like a team of superheroes, each with its own special powers but constantly communicating and supporting one another. Here’s how they work together:
The Gut: Home to trillions of bacteria, fungi, and other microbes, your gut is a powerhouse of activity. It helps digest food, produces vitamins, and even trains your immune system.
The Brain: The brain is the command center, sending signals to the gut and liver through nerves and hormones. It also responds to signals from these organs, like when your gut feels “off” and you get a headache or feel anxious.
The Liver: The liver is the body’s detox machine. It filters out toxins, processes nutrients, and helps regulate inflammation. It’s also a key player in your immune system.
When these three are in sync, everything runs smoothly. But when something goes wrong—like an imbalance in gut bacteria, liver stress, or brain inflammation—it can throw the whole system off balance, and your lungs can suffer as a result.
How the Gut-Brain-Liver Axis Affects the Lungs
The lungs might seem far removed from your gut or liver, but they’re actually deeply connected through something called the gut-lung axis. This phenomenon refers to how the gut microbiome—including the gut mycobiome (the fungal component)—can influence immunity and health in distant organs. In this article, we’re focusing on the lungs and how this intricate connection impacts your breathing.
1. Gut Imbalances and Lung Health
Your gut is home to a diverse community of microbes, and when this community gets out of balance (a condition called dysbiosis), it can affect your lungs. For example:
Inflammation: An unhealthy gut can send out inflammatory signals that travel through your bloodstream to your lungs, making conditions like asthma or COPD worse.
Weakened Immunity: A balanced gut microbiome helps train your immune system to fight off infections. When it’s out of whack, you might be more prone to respiratory infections like the flu or pneumonia.
2. The Brain’s Role in Lung Function
Your brain and lungs are in constant communication through the vagus nerve, a major nerve that connects the two. Stress, anxiety, or inflammation in the brain can affect how well your lungs work. For example:
Stress and Breathing: Ever noticed how stress makes it harder to breathe? That’s your brain-lung connection at work. Chronic stress can even worsen conditions like asthma.
Brain Inflammation: Inflammation in the brain (often linked to gut imbalances) can send signals that increase inflammation in the lungs, making it harder to breathe.
3. The Liver’s Impact on the Lungs
The liver is your body’s detoxifier, but it also plays a big role in regulating inflammation. When the liver is stressed—say, from a poor diet, alcohol, or toxins—it can’t do its job as well. This can lead to:
Toxic Buildup: If the liver isn’t filtering toxins properly, they can build up in your bloodstream and affect your lungs, leading to inflammation or even lung damage.
Immune Dysfunction: The liver helps regulate your immune system. If it’s not functioning well, your body might overreact to infections, causing more harm than good.
Lung Inflammation: A stressed liver can release inflammatory substances into the bloodstream, which travel to the lungs and cause inflammation. Over time, this can damage lung tissue and make breathing harder, especially in people with liver disease.
But here’s the twist: the connection between the liver and lungs is two-way. Just as liver dysfunction can harm the lungs, lung problems can also stress the liver. For example:
Lung Damage: Severe lung issues can reduce oxygen levels, trigger widespread inflammation, and disrupt blood flow, all of which strain the liver.
Liver Conditions: People with chronic liver problems are more prone to lung complications, creating a vicious cycle where damage in one organ worsens the other.
In short, the liver and lungs are deeply connected. Keeping one healthy helps protect the other, while problems in one can quickly spiral into issues for both.

When Things Go Wrong: Examples of Lung Problems Linked to the Axis
Imbalances in the gut-brain-liver axis can contribute to a variety of lung issues. Here are a few examples:
1. Asthma
Research shows that people with asthma often have different gut bacteria compared to those without the condition. An imbalanced gut microbiome can trigger inflammation in the lungs, making asthma symptoms worse.
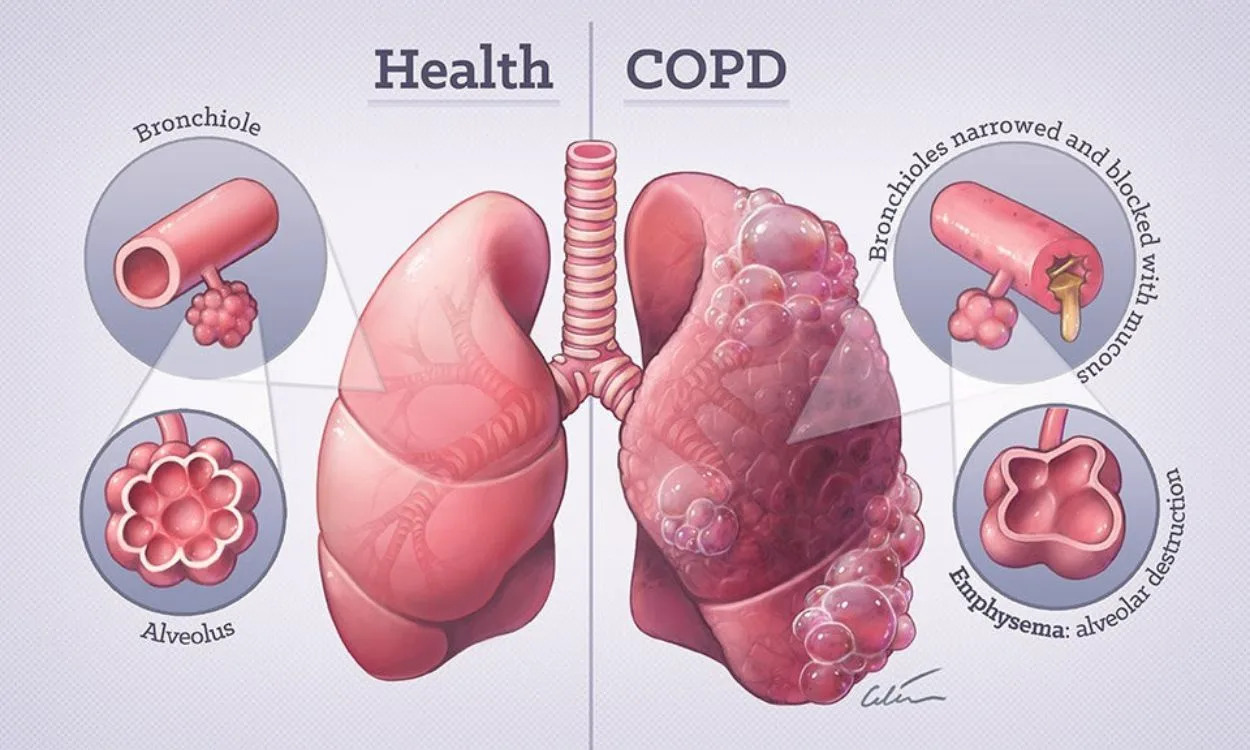
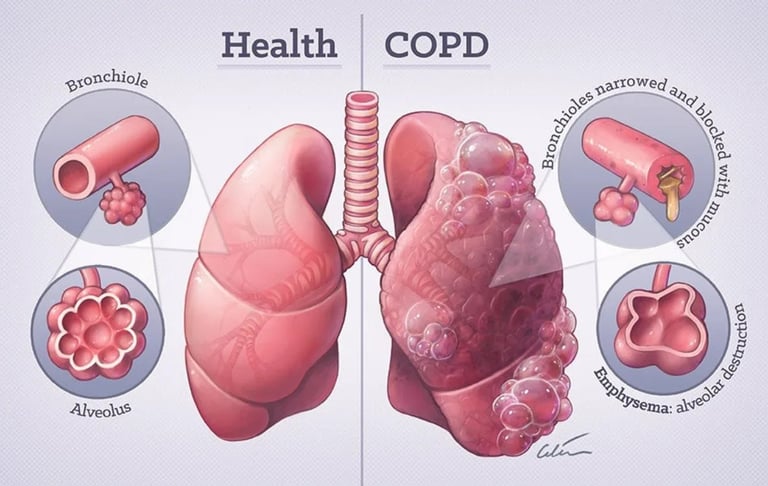
2. Chronic Obstructive Pulmonary Disease (COPD)
COPD is a lung disease often caused by smoking, but gut and liver health play a role too. A stressed liver—whether from poor diet, toxins, or conditions like NAFLD (Non-Alcoholic Fatty Liver Disease)—can’t filter toxins as effectively, leading to more inflammation in the lungs. Meanwhile, gut imbalances can weaken the immune system, making it harder to fight off infections that worsen COPD.
3. Respiratory Infections
Your gut microbiome helps train your immune system to fight off viruses and bacteria. When it’s out of balance, you’re more likely to get sick—and stay sick longer. This is especially true for respiratory infections like the flu or even COVID-19. But it doesn’t stop there. A disrupted gut can also lead to chronic cough and a weakened chest long after the infection is gone. Here’s how:
Prolonged Infections: A weakened immune system can’t clear infections as effectively, leading to lingering symptoms like a persistent cough.
Chronic Inflammation: Gut imbalances can cause ongoing inflammation in the lungs, making your airways hypersensitive and triggering a cough even when there’s no active infection.
Excess Mucus: An unhealthy gut can lead to overproduction of thick, sticky mucus in the lungs, making it harder to breathe and leaving your chest feeling heavy or weak.
4. Acute Respiratory Distress Syndrome (ARDS)
ARDS is a severe lung condition that can happen after an infection or injury. The liver plays a key role in regulating inflammation during ARDS, and if it’s not functioning well, the condition can become even more serious.



The Big Picture: Your Body Is a Connected System
Your lungs don’t exist in isolation—they’re part of a complex, interconnected system that includes your gut, brain, and liver.
When one part of this system is out of balance, it can ripple through your body and affect your breathing.
By taking care of your gut, brain, and liver, you’re not just supporting these organs—you’re also giving your lungs the best chance to stay healthy and strong.
Most “dis-eases” start with small nudges—little red flags like a lingering cough, fatigue, or a feeling that something’s off.
If you ignore these signs, thinking they’ll go away on their own, you’re setting yourself up for a bigger problem down the road.
Medications might help manage symptoms, but they won’t restore balance to your gut-brain-liver axis.
What you need is a holistic approach—one that addresses the root causes and supports your body’s natural ability to heal. Consider adding pure, high-quality supplements to your routine.
If you keep brushing off those red flags, your body will eventually reach its breaking point.
We don’t know when the bulldozer will hit—it could be anytime, when the conditions are just right (or wrong). Chronic illness, severe symptoms, or even organ damage could be the result.
So, listen to your body. Pay attention to the small signs now.
Return to:
