GERD: More Than Just Heartburn!
Gastroesophageal reflux disease (GERD) is primarily a digestive issue, but its effects go beyond the gut, impacting the brain and liver through interconnected networks. The gut-brain axis, a communication link between the gut and central nervous system, explains how disruptions like GERD can influence mood and mental health. For example, GERD has been associated with increased anxiety and depression, partly due to the vagus nerve's role in relaying gut signals to the brain, which can affect emotional well-being.
Similarly, the gut-liver axis plays a crucial role in managing systemic inflammation and metabolism. Impaired liver function due to chronic inflammation can worsen GERD, as the liver's role in detoxification and digestion becomes compromised. This creates a cycle where liver dysfunction exacerbates gut issues, including reflux. Together, these systems—the gut, brain, and liver—form a complex network that significantly impacts conditions like GERD.
It’s important to differentiate occasional heartburn from GERD. If infrequent heartburn becomes a regular occurrence, it may signal the presence of GERD, necessitating evaluation by a healthcare professional.
The Hidden Players: Muscles, Nerves, and Mucosa
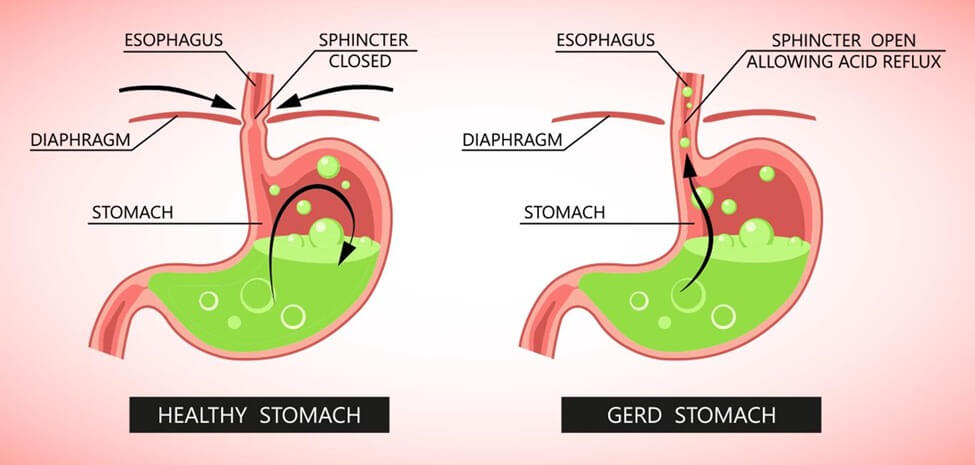
A common misconception about GERD is that it’s caused by an excess of stomach acid. In reality, prevailing scientific research shows that GERD primarily arises from a dysfunction of the lower esophageal sphincter (LES), the muscle that separates the stomach from the esophagus. When the LES is functioning correctly, it opens only to allow swallowed food and liquids to pass into the stomach and to release gas during burping. Unfortunately, if the LES is weak or not working properly, it can permit stomach acid to escape into the esophagus, leading to irritation and discomfort.
At the core of this issue often lies a complex interplay of muscles, nerves, and the mucosal lining surrounding the esophagus and stomach. The stomach’s mucosa plays a crucial role in protecting the inner lining from the acidic environment necessary for digestion. When the mucosal barrier is weakened—due to conditions like atrophic gastritis, where the gastric mucosa thins—the stomach becomes more vulnerable to irritation and inflammation. This can further exacerbate GERD symptoms.
The nerves that control the LES are closely linked to overall digestive health. But here’s the twist—stress plays a significant role in this relationship. Stress can disrupt the function of the LES and also impact the stomach muscles, which are crucial for pushing food into the small intestine. Additionally, when the mucosal barrier is compromised, the stomach lining may struggle to manage the acidic content, leading to increased discomfort. Therefore, symptoms like heartburn, gastritis, and GERD can arise from a multitude of factors working together, rather than simply from dietary triggers.
The Gut-Liver-Brain Axis: Where it All Connects
To tackle GERD holistically, it's vital to understand how the gut, liver, and brain are interconnected. Stress from the brain, often linked through the vagus nerve, can influence digestive function, making the LES more likely to relax at the wrong time. Additionally, the liver plays a significant role by producing bile, essential for fat digestion. If the liver is sluggish, often due to chronic inflammation, bile production and detoxification can suffer, worsening digestive symptoms like reflux. Essentially, GERD isn’t just about acid; it’s about a disrupted system involving digestion, stress, and detoxification.
A Holistic Approach to GERD
Rather than just addressing symptoms with acid-reducing pills, focusing on healing the gut-liver-brain axis can provide longer-lasting relief.
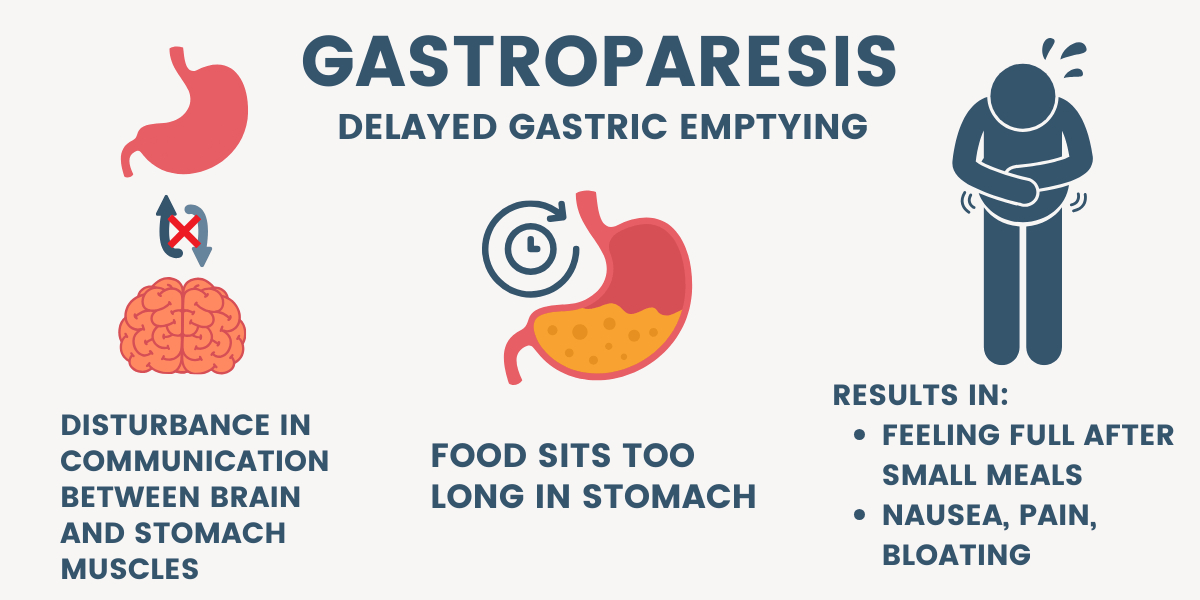
Support the Gut: A healthy gut can be maintained through fiber-rich foods, probiotics, and prebiotics like inulin (chicory root). These help protect the gut lining, improving overall digestion. Soluble fiber plays a vital role by protecting the gut lining and promoting the growth of beneficial bacteria, improving overall digestion. However, for those with sensitivities, consuming large amounts of soluble fiber can delay gastric emptying and trigger GERD symptoms.
On the flip side, while insoluble fiber helps promote regular bowel movements, it may cause discomfort for some, particularly if they have sensitive digestive systems. For individuals with GERD, it’s crucial to pay attention to how both types of fiber affect them. Striking the right balance can enhance gut health while reducing the risk of GERD flare-ups.
Liver Support: Leafy greens, bitters such as turmeric, picao preto, and milk thistle can help support liver function and improve bile production, aiding digestion and reducing reflux. Additionally, minimizing exposure to contaminants and pollution is vital for overall health; what we eat, drink, and inhale can all impact our well-being. Opting for organic foods when possible—and ensuring that any supplements we take are pure and safe—can help bolster the body’s detoxification processes.
Brain Balance: Stress management is key. Techniques like meditation, deep breathing, and gentle exercise help reduce stress, keeping your nerves and muscles calm and functioning properly. Adaptogens like ashwagandha, cistanche tubulosa, eleuthero, and ginkgo biloba also support stress reduction and help regulate the gut-brain connection. By managing stress, you’re giving your body the best chance to restore balance and improve digestion.
Get Enough Protein: Protein isn’t just for muscles; it supports the cells in your gut lining, helping heal and strengthen the LES and gut. It also balances stomach acid production by buffering excess acid, reducing damage to the stomach and esophagus. In particular, glutamine—a key amino acid—nourishes the mucosal lining, promoting healing and reducing inflammation.
Note: While the body normally produces enough glutamine in tissues like muscles, lungs, and the liver, high physical stress—such as illness, injury, infection, or intense exercise—can increase the body's demand. In these situations, natural production may not keep up, depleting glutamine stores. Supplements can help replenish these reserves when necessary.
Focusing on the Axis, Not Just Pills
While antacids and other medications can relieve symptoms temporarily, long-term use may lead to deficiencies in essential nutrients like magnesium, which is vital for muscle function—including the lower esophageal sphincter (LES). It's crucial to remember that heartburn and GERD are not solely due to excess stomach acid; low stomach acid can also contribute to these conditions. By targeting the root causes of GERD through gut, liver, and brain health, you can reduce reliance on medications and support your body’s natural healing processes. Addressing stress, diet, and overall gut health is a more effective approach than merely treating symptoms. This holistic perspective allows for a deeper understanding of your digestive health and can lead to more effective management of GERD.
Key Takeaways:
Dysfunction of the LES: GERD primarily arises from dysfunction of the lower esophageal sphincter, not just excess stomach acid.
Acid Balance: Both low and high stomach acid levels can contribute to GERD, emphasizing the need for balance.
Interconnected Systems: A disrupted system involving digestion, stress, and detoxification is at play, highlighting the importance of a comprehensive approach to gut, liver, and brain health.
While we may discuss the gut, liver, and brain as distinct systems for clarity, it’s essential to remember that they are not truly separate; they are intricately interconnected. Disruptions in one system can significantly impact the others. For instance, stress can impair digestive function, while an unhealthy gut can negatively affect liver detoxification and brain health. This interconnectedness underscores the importance of a holistic approach, as nurturing one system helps restore balance and supports the overall well-being of the entire body.
Of course, it’s vital to be mindful of lifestyle factors that could hinder your body’s remarkable healing mechanisms. Poor dietary choices, lack of sleep, chronic stress, excessive alcohol consumption, tobacco use, and overeating can all create roadblocks for your digestive system. Implementing small changes, like incorporating more whole foods, practicing stress-relief techniques, moderating alcohol intake, quitting smoking, and being mindful of portion sizes, can significantly enhance your body’s natural ability to heal. After all, your body is quite remarkable at taking care of itself when given the right support!
Disclaimer: The information provided in this article is not intended to diagnose, treat, cure, or prevent GERD or any other medical condition. The focus here is on supporting the body’s systems holistically through diet, stress management, and natural supplements. If you have concerns about GERD or other health conditions, consult a healthcare professional for personalized advice.
Return to:




